Blog
Learn all you need to know about Louisiana Medicare Plans, Medigap, Medicare Supplement, and Medicare Advantage Plans.
Does Medicare Advantage Cover Pre Existing Conditions?
This article provides an introduction to Medicare Advantage coverage of pre-existing conditions, including the understanding of pre-existing conditions in healthcare insurance, coverage rules and limitations, enrollment and waiting periods, out-of-pocket costs and financial considerations, as well as providing assistance and resources for individuals navigating Medicare Advantage coverage for pre-existing conditions.
Introduction to Medicare Advantage Coverage of Pre-existing Conditions
Understanding how Medicare Advantage Plans address pre-existing conditions is paramount for individuals seeking comprehensive healthcare coverage. Pre-existing conditions encompass a wide range of health issues that individuals have before enrolling in a health insurance plan, such as chronic illnesses, past surgeries, or ongoing health concerns. For instance, individuals with diabetes or heart disease may require specialized care and medications to manage their conditions effectively.
By delving into the specifics of how Medicare Advantage Plans cater to pre-existing conditions, individuals can make informed decisions about their healthcare coverage. These plans, also known as Medicare Part C, accept individuals with pre-existing conditions and offer benefits like vision, dental, and [prescription drug coverage]. Medicare Advantage Plans allow enrollment with pre-existing conditions, but caution is advised. For example, a person with arthritis may benefit from a Medicare Advantage Plan that covers both medical treatments and physical therapy sessions to alleviate pain and improve mobility. Therefore, gaining insights into how these plans handle pre-existing conditions is crucial for individuals to access the necessary care and support for their health needs.
Understanding Pre-existing Conditions in Healthcare Insurance
When we talk about pre-existing conditions in the context of healthcare insurance, we refer to health issues that exist before enrolling in a health insurance plan. These conditions can range from chronic illnesses like diabetes or heart disease to prior surgeries or ongoing health concerns. For individuals with pre-existing conditions, obtaining traditional health insurance coverage can be challenging due to potential denials, higher premiums, or benefit limitations.
For instance, let's consider a scenario where an individual has diabetes, a common pre-existing condition. Before the Affordable Care Act, this individual might have struggled to find adequate health insurance coverage that included their diabetes care without facing exorbitant costs. However, Medicare Advantage Plans have been instrumental in addressing these concerns. They accept individuals with pre-existing conditions and offer a wide array of benefits, such as vision, dental, and prescription drug coverage, tailored to meet the unique healthcare needs of individuals with pre-existing conditions.
Coverage Rules and Limitations under Medicare Advantage Plans
Medicare Advantage Plans not only accept individuals with pre-existing conditions but also offer a wide range of benefits to enhance their healthcare coverage. For instance, these plans may include vision, dental, and prescription drug coverage, which are not typically provided by Original Medicare. This expanded coverage under Medicare Advantage aims to address the diverse healthcare needs of beneficiaries with pre-existing conditions, ensuring comprehensive care and support.
In contrast to some insurance plans like Medicare Supplement Plans that may enforce waiting periods or charge higher premiums for individuals with pre-existing conditions, Medicare Advantage Plans stand out for their inclusive approach to coverage. By focusing on providing accessible and comprehensive healthcare benefits, Medicare Advantage Plans aim to bridge gaps in coverage for those with pre-existing conditions. This commitment to offering extensive coverage without waiting periods or heightened costs demonstrates the dedication of Medicare Advantage Plans to prioritize the well-being of individuals with pre-existing conditions. It is crucial for potential beneficiaries to thoroughly assess the specifics of each Medicare Advantage Plan, considering factors like networks, copayments, and prescription drug coverage, to make an informed decision that best suits their healthcare requirements.
Enrollment and Waiting Periods for Medicare Advantage Plans
Enrolling in a Medicare Advantage Plan is a pivotal step for individuals with pre-existing conditions to secure comprehensive healthcare coverage. The Annual Enrollment Period stands out as a crucial window during which beneficiaries can carefully assess various plan options, weighing factors like coverage for pre-existing conditions, prescription drugs, and additional benefits. This period empowers individuals to make informed choices tailored to their specific health needs, ensuring that pre-existing conditions are adequately covered without unexpected limitations.
Moreover, Medicare Advantage Plans prioritize transparency regarding waiting periods and coverage constraints linked to pre-existing conditions. By providing clear information on these aspects, beneficiaries can navigate the enrollment process with confidence, knowing the extent of coverage available and any potential waiting periods that might apply. This transparency fosters trust between individuals and their chosen Medicare Advantage Plan, offering peace of mind and clarity when managing pre-existing health concerns within the healthcare system.
Out-of-pocket Costs and Financial Considerations
When considering Medicare Advantage Plans, individuals with pre-existing conditions should pay attention to the out-of-pocket costs associated with these plans. These costs play a crucial role in determining the overall affordability and financial impact of healthcare coverage. For instance, Medicare Advantage Plans often establish out-of-pocket maximums, which serve as a financial safety net by capping the total amount individuals with pre-existing conditions may have to pay for covered services in a given plan year. This feature provides predictability and peace of mind, especially for those managing chronic health issues.
Moreover, beyond the out-of-pocket maximums, it is essential for beneficiaries to delve into the specifics of copayments and coinsurance associated with different Medicare Advantage Plans. These cost-sharing components can significantly influence the overall financial burden on individuals with pre-existing conditions. For example, a plan with lower copayments for specialist visits or a reduced coinsurance rate for prescription medications might be more financially advantageous for someone with specific healthcare needs. Therefore, a detailed comparison of these costs can empower individuals to make informed decisions regarding the most suitable Medicare Advantage Plan for their medical and financial requirements.
We're Here to Help
Bourgeois Insurance Agency Medicare covers pre-existing conditions immediately, including under Medicare Advantage Plans, but Medigap policies may have a waiting period or denial for pre-existing conditions. By specializing in Medicare Advantage, Medicare Supplement, Life Insurance, Health Insurance, Auto & Home Insurance, and more, Bourgeois Insurance Agency brings a wealth of knowledge and experience to guide clients effectively. For instance, they offer free consultations that provide personalized insights to help individuals comprehend their Medicare coverage options thoroughly. This tailored approach ensures that individuals with pre-existing conditions receive the necessary support to navigate the complexities of insurance and make well-informed decisions.
Moreover, Bourgeois Insurance Agency's commitment to assisting individuals with pre-existing conditions extends to facilitating the entire process of finding the right insurance coverage. By offering free consultations and personalized guidance, they empower clients to navigate the intricacies of Medicare Advantage Plans with ease. Whether through a phone call at (985) 803-8999 or a visit to their website, individuals seeking assistance in understanding and selecting Medicare Advantage Plans tailored to their needs can benefit from Bourgeois Insurance Agency's comprehensive support and expertise. For those navigating the landscape of healthcare insurance with pre-existing conditions, Bourgeois Insurance Agency remains a reliable partner in making informed and beneficial choices for their coverage needs.
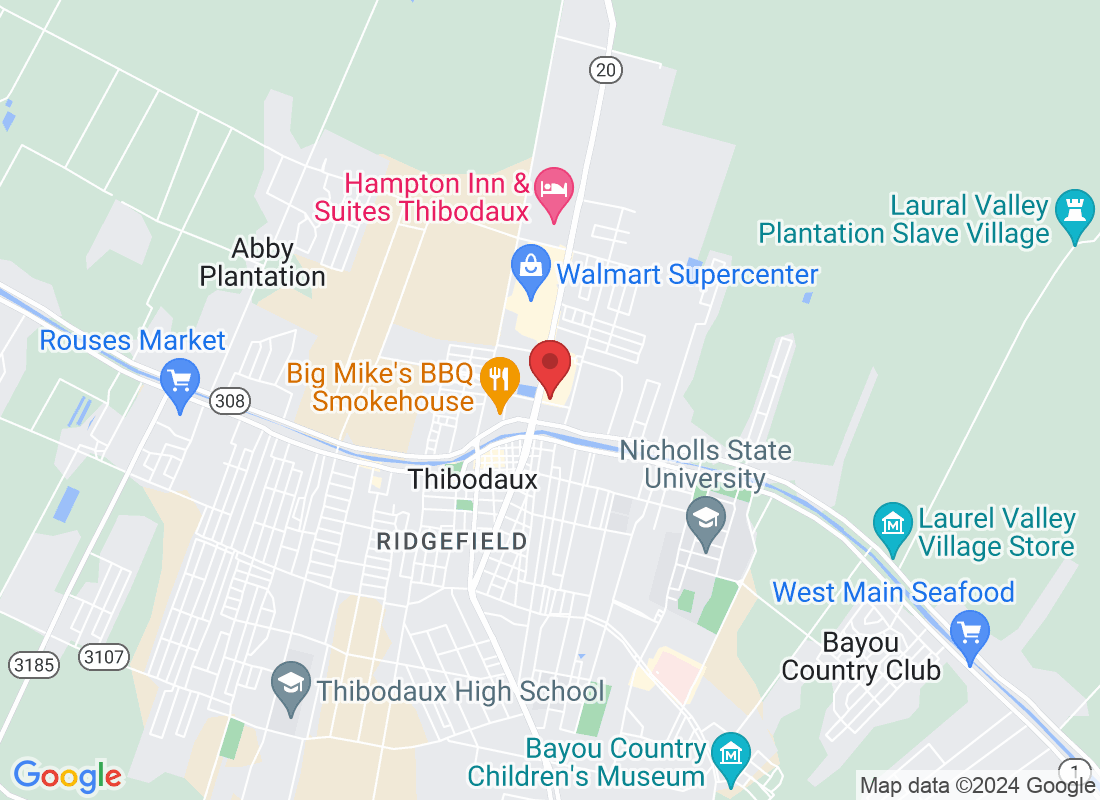
Address
Office Address
311 N Canal Blvd Thibodaux, LA 70301
Email Address
Office Number
(985) 803-8999
Resources
Contact Us
Address:
311 N Canal Blvd Thibodaux, LA 70301
Plans are insured or covered by Medicare Advantage (HMO, PPO, and PFFS) organization with a Medicare contract and/or a Medicare-approved Part D sponsor. Enrollment in the plan depends on the plan’s contract renewal with Medicare. We do not offer every plan in your area. Please contact medicare.gov or 1-800-Medicare to get information on all your options.
Bourgeois Insurance Copyright 2023 --
All Rights Reserved --