Blog
Learn all you need to know about Louisiana Medicare Plans, Medigap, Medicare Supplement, and Medicare Advantage Plans.
Why Do Doctors Not Like Medicare Advantage Plans?
Doctors discontent with Medicare Advantage Plans stems from frustrating claim denials, limitations and unexpected costs, as well as challenges in balancing patient care needs with plan restrictions, potentially impacting patient care and creating financial and administrative challenges.
The adoption of Medicare Advantage Plans among seniors has been steadily increasing, with over half of all Medicare beneficiaries opting for these plans. While these plans offer comprehensive coverage and additional benefits such as vision and dental care, doctors are increasingly expressing discontent with certain aspects of Medicare Advantage Plans. Understanding the reasons behind doctors' hesitance towards these plans is essential for patients and healthcare providers to navigate the complexities of the healthcare system effectively.
Physicians and hospitals' dissatisfaction with Medicare Advantage Plans stems from various factors, including the high number of claim denials and the cumbersome preapproval requirements imposed by these plans. For example, a recent study by the Health and Human Services Department's inspector general revealed that over 35 million prior approval requests were submitted for Medicare Advantage enrollees in the last 3 years, highlighting the administrative burden faced by healthcare providers. These challenges not only impact the efficiency of care delivery but also raise concerns about the quality of patient care under Medicare Advantage Plans.
Reasons for Doctor Discontent with Medicare Advantage Plans
Physicians and hospitals often express dissatisfaction with Medicare Advantage Plans due to the high number of claim denials and complex preapproval requirements. The limitations and unexpected costs associated with these plans can impact the quality of care that doctors can deliver. Moreover, navigating the restrictions, referral demands, and out-of-pocket costs of Medicare Advantage Plans poses challenges for healthcare providers in balancing patient care needs.
One key reason some doctors prefer not to accept Medicare Advantage Plans is the difference in payment rates compared to traditional Medicare. Medicare Advantage Plans, also known as Medicare Part C, often have lower reimbursement rates for healthcare providers than Original Medicare, which can lead to financial strain on medical practices and hospitals. This disparity in payment rates can make it less appealing for doctors to participate in Medicare Part C networks, affecting their willingness to accept patients with these plans.
Furthermore, the prior approval requirements in Medicare Advantage Plans can significantly impact the efficiency of care delivery by adding administrative burdens to healthcare providers. The need for preauthorization for certain treatments or procedures can delay patient care, leading to frustration among both doctors and patients. This additional paperwork and approval process can divert valuable time and resources away from direct patient care, contributing to the discontent felt by healthcare providers towards Medicare Advantage Plans.
Impact on Patient Care
The impact on patient care due to doctors' reluctance to accept certain Medicare Advantage Plans goes beyond mere inconvenience. Patients who have developed trusted relationships with specific healthcare providers may find themselves facing restricted access when these providers choose not to participate in certain Advantage plans. For example, a patient who has been seeing a specialist for a chronic condition may suddenly have to switch to a different provider within the plan's network, disrupting the continuity and quality of care they were receiving.
Moreover, the denial of coverage for necessary care and prescription drugs under certain Medicare Advantage Plans can have serious consequences for patient health outcomes. Imagine a scenario where a patient enrolled in a Medicare Advantage Plan requires a specific medical procedure that is deemed essential by their healthcare provider but is denied coverage, significantly affecting the patient's out-of-pocket costs. This denial not only delays the necessary treatment but can also lead to exacerbated health conditions or prolonged suffering for the patient.
Furthermore, the departure of medical groups from the networks of certain Advantage insurers due to inadequate coverage for patient care highlights significant gaps in healthcare accessibility for patients. This situation can leave patients scrambling to find alternative providers within their plan's network, potentially facing longer wait times for appointments or having to travel greater distances to receive care. Ultimately, these disruptions and limitations in access can impact the overall well-being and satisfaction of patients relying on Medicare Advantage Plans for their healthcare needs.
Financial and Administrative Challenges
Healthcare providers encounter various financial and administrative challenges when dealing with Medicare Advantage Plans. One significant concern is the high denial rates and delayed payments that can strain the financial stability of medical practices. For instance, providers facing frequent claim denials may experience cash flow disruptions, affecting their ability to cover operational costs and invest in quality patient care.
Moreover, the dissatisfaction among healthcare providers with Medicare Advantage Plans is exacerbated by the cumbersome prior authorization processes and allegations of billing fraud. These issues not only create administrative burdens for medical practices but also contribute to increased frustration among providers, hindering the efficiency of care delivery. For example, the time and resources spent on navigating complex preapproval requirements can divert attention from direct patient care, impacting overall practice productivity.
Additionally, tensions arise from negotiation tactics surrounding payment rates and preapproval mandates within Medicare Advantage Plans. The discrepancies in reimbursement rates and the stringent preapproval criteria set by insurers can create financial uncertainties for healthcare providers. This can lead to challenges in budget planning and resource allocation, affecting the long-term sustainability of medical practices, especially with the unpredictability of Medicare coverage. As a result, providers may find themselves grappling with financial decisions that impact both their bottom line and the quality of care they can offer to patients.
Policy and Regulatory Responses
In response to the growing concerns raised by healthcare providers regarding Medicare Advantage Plans, the Biden administration has taken steps to address these issues. One significant action has been the implementation of rules that mandate Medicare Advantage Plans to provide care that is equivalent in terms of medical necessity to what traditional Medicare offers. This move aims to ensure that patients enrolled in Medicare Advantage Plans receive the same level of care and rights as those under the traditional Medicare program, thereby upholding standards of care quality and patient rights.
Furthermore, the Centers for Medicare & Medicaid Services (CMS) has proposed additional regulations aimed at improving transparency and accountability within Medicare Advantage Plans. These regulations focus on areas such as broker commissions and the transparency of prior approval programs. By enhancing oversight and transparency, CMS strives to protect the interests of both beneficiaries and healthcare providers within the Medicare Advantage system. These regulatory measures are designed to promote fairness, efficiency, and clarity in the administration of Medicare Advantage Plans, ultimately benefiting both patients and healthcare providers.
Additionally, the American Hospital Association has been actively advocating for robust oversight by CMS in response to the new rules governing Medicare Advantage Plans. This advocacy underscores the ongoing commitment to maintaining high standards of patient care and protecting the interests of healthcare providers. By calling for rigorous oversight, the American Hospital Association aims to ensure that Medicare Advantage Plans operate in a manner that upholds the quality of care, patient rights, and the financial sustainability of healthcare providers. These collaborative efforts between regulatory bodies and healthcare organizations demonstrate a shared commitment to addressing challenges within the Medicare Advantage system and promoting positive outcomes for all stakeholders.
We're Here to Help
When healthcare providers encounter challenges with Medicare Advantage Plans, seeking expert guidance can be crucial to navigating the complexities effectively. Bourgeois Insurance Agency, LLC stands out as a reliable source of assistance for those looking to understand the intricacies of insurance options, especially regarding Medicare Advantage and Medicare Supplement plans. By offering free consultations, Bourgeois Insurance ensures that clients receive personalized recommendations tailored to their specific needs and preferences.
Moreover, Bourgeois Insurance's commitment to providing comprehensive consultation services goes beyond basic insurance offerings, including advice on enrollment in Medicare Advantage (Part C) and prescription drug plans. By addressing the unique concerns and preferences of each client, the agency ensures that healthcare providers have access to the information and support necessary to navigate the evolving landscape of Medicare Advantage Plans effectively. For healthcare professionals seeking clarity on insurance options and wanting to optimize their coverage choices, Bourgeois Insurance's expertise and resources can serve as valuable assets in making well-informed decisions. Visit bourgeoisinsurance.com to explore how expert guidance can streamline your insurance decision-making process and enhance your practice's financial stability and patient care outcomes.
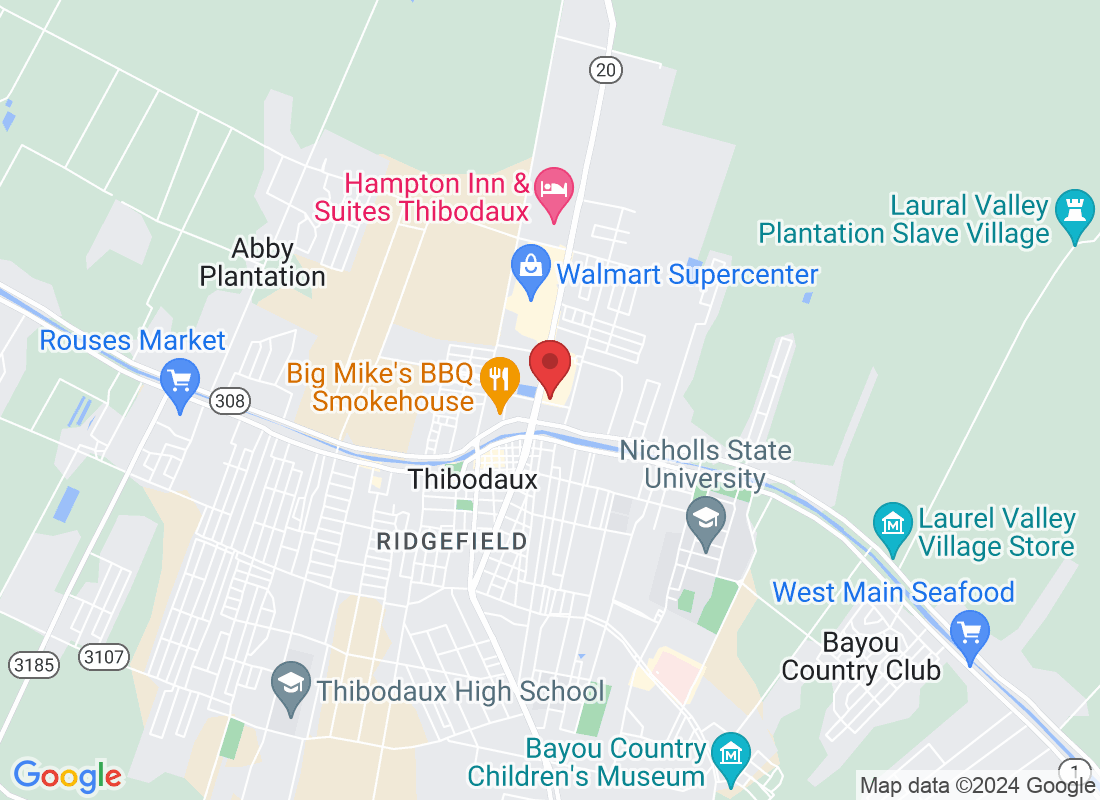
Address
Office Address
311 N Canal Blvd Thibodaux, LA 70301
Email Address
Office Number
(985) 803-8999
Resources
Contact Us
Address:
311 N Canal Blvd Thibodaux, LA 70301
Plans are insured or covered by Medicare Advantage (HMO, PPO, and PFFS) organization with a Medicare contract and/or a Medicare-approved Part D sponsor. Enrollment in the plan depends on the plan’s contract renewal with Medicare. We do not offer every plan in your area. Please contact medicare.gov or 1-800-Medicare to get information on all your options.
Bourgeois Insurance Copyright 2023 --
All Rights Reserved --